Diabetes in Dogs: Causes, Signs, & Care (Vet Answer)

Updated on

Click to Skip Ahead
Diabetes mellitus (DM) is a common endocrinopathy or hormonal condition in dogs, particularly in the 7–10-year age group. The condition is also more common (approximately twice as much) in female dogs than males. Several studies have identified various dog breeds that are at increased risk for developing diabetes mellitus and also others that have an apparent reduced risk. Such disease incidence is likely heavily influenced by geographical area and breed preference.
Unfortunately, the management of diabetic dogs can, in some cases, be quite frustrating. Often there is a need to adjust the treatment plan, particularly in cases where there is insulin resistance, requiring a higher insulin dose to manage the clinical signs. Below, we’ll go over some common clinical signs of this condition in dogs, how to manage them, and why treatment can become more complicated.
What Is Diabetes?
There are two categories of diabetes in dogs: diabetes mellitus and diabetes insipidus. While both conditions cause increased water intake and excessive urination, it is crucial to distinguish between them because the potential causes for each differ significantly, and the two conditions require vastly different treatments.
Diabetes mellitus refers to a persistently elevated blood level. In diabetes insipidus, the blood glucose levels are normal, and the condition is characterized by excessive urination and associated increased thirst because of impaired salt and water metabolism. For this article, we’ll focus on diabetes mellitus alone, and any use of the term “diabetes” below is about diabetes mellitus.

What Are the Signs of Diabetes?
The hallmark signs of diabetes include increased water intake (referred to as polydipsia), increased urination (or polyuria), an increased appetite (also known as polyphagia), and, often, concurrent weight loss. Not all diabetic dogs have an increased appetite at the time of presentation, and its absence should prompt further investigation into concurrent diseases or complications of diabetes that would affect its management.
While the above clinical signs are typically what owners of diabetic dogs notice or even prompt them to take their beloved friend to the local veterinary clinic, they are not the only changes that may be seen with diabetes in dogs. Unfortunately, the development of cataracts is also common in diabetic dogs, with some studies suggesting that approximately 80% of diabetic dogs will develop cataracts within the first year of being diagnosed. As is the case in humans, cataracts can significantly negatively impact vision.
Other clinical signs that can be seen are those related to either a complication of inadequate management (e.g., diabetic ketoacidosis (DKA)) or those attributable to underlying disease processes that have brought about insulin resistance and precipitated, for instance, DKA. Dogs suffering from DKA may have clinical signs including any combination of the following: inappetence/anorexia, vomiting, signs of weakness, and dehydration. As alluded to above, such cases are complicated and require further work-up to determine what led to the progression to this state.
Clinical signs related to underlying disease processes might include skin and coat changes with hyperadrenocorticism (Cushing’s disease) or inappetence, vomiting, and abdominal pain associated with pancreatitis, to mention a few more common culprits.
What Are the Causes of Diabetes?
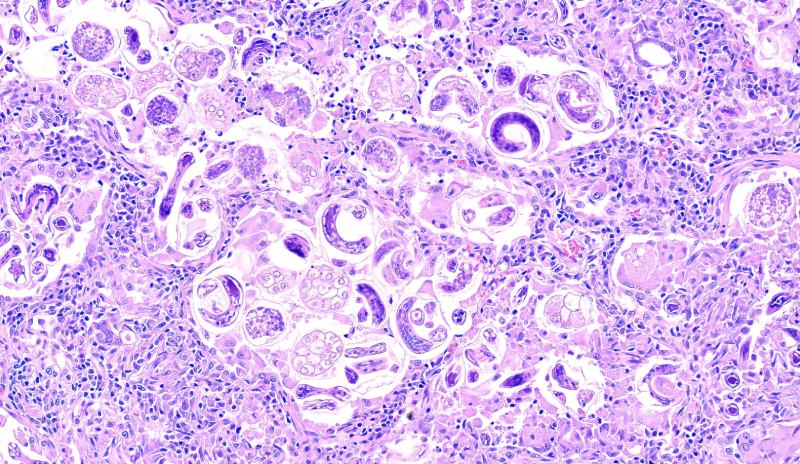
Diabetes mellitus results from a deficit in insulin production, its action at the cellular level, or both. Underlying mechanisms for its development include genetics, possible environmental factors, the presence of pancreatic disease, conditions (or use of drugs) causing insulin resistance, and potentially, an autoimmune disorder targeting the specific cells (beta-cells) in the pancreas responsible for insulin production.
As mentioned above, various dog breeds have been identified as being at increased risk of developing diabetes mellitus. It has been proposed that breed susceptibility is associated with immune-response genes. In other words, at-risk breeds are more likely to have an autoimmune condition resulting in beta-cell destruction and decreased insulin production.

How Do I Care for a Dog With Diabetes?
As with most medical conditions, treat the underlying cause whenever possible. This is most important in cases of diabetes believed to be transient in nature, meaning it’s associated with the use of certain drugs or medical conditions that affect the action of insulin.
Treating a diabetic dog requires insulin administration in the form of a subcutaneous or under-the-skin injection. Regarding the different insulin options available, these can broadly be categorized as rapid-acting, intermediate-acting, and long-acting.
Generally speaking, the rapid-acting variety is reserved for in-hospital use, particularly with managing extremely high blood glucose associated with complications such as DKA. Intermediate-acting insulins are often the mainstay of therapy in the chronic management of diabetic dogs. While insulin response is highly variable among patients, typically, most intermediate-acting insulins need to be administered twice daily.
With further advancements in managing diabetes in humans came the development of long-acting and even ultra-long-acting insulins, which, in some patients, may require anywhere from once daily to even once weekly injections. Despite their classification, these long-acting formulations often still require twice daily administration for the most effective control of blood glucose levels. Ultra-long-acting insulins are still relatively new but could potentially change the way diabetic dogs are managed in the not-too-distant future, so watch this space!
Diet and feeding practices are also crucial for the management of diabetic dogs. Such dogs should be fed two equal-sized meals twice daily, each given just before the scheduled insulin injection. Typically, a high-fiber diet is recommended.
The use of a continuous glucose monitor (CGM) can be beneficial for monitoring glucose levels in diabetic dogs and can also help guide insulin dosage adjustments to ensure that hypoglycemia (too low of a blood sugar level) is avoided. A CGM is a small sensor applied on the surface of a dog’s skin and can measure interstitial glucose, which serves as a fairly accurate marker of blood glucose levels.
While such tools can be helpful in decision-making when it comes to adjusting insulin dose, it is essential to remember that the most valuable tool when it comes to decision-making is the clinical picture. In other words, are the clinical signs of increased water intake, excessive urination, and an increased appetite controlled or significantly improved? If the answer is yes, then it’s probably not necessary and potentially even harmful to try to chase perfect/normal blood glucose levels.
Consistency is key when managing a diabetic dog regarding diet, exercise, and insulin administration.
Frequently Asked Questions
What Are the Types of Diabetes in Dogs?
Various types of diabetes have been described in humans, and such distinctions and terminology have more or less been transcribed to our canine friends. In dogs, the most common form of diabetes resembles that referred to as type 1 DM. Previously, type 1 DM was known as insulin-dependent DM because it is characterized by a permanent state of insulin deficiency. Therefore, such patients have an absolute need for exogenous (injectable) insulin to manage blood glucose levels and prevent unwanted and often life-threatening complications of untreated diabetes, such as ketoacidosis and even death.
Transient or reversible diabetes is extremely uncommon to even rare in dogs. It is typically diagnosed in dogs that were previously subclinical diabetics and have either another medical condition or are being administered a drug that is bringing about insulin antagonism or resistance. Type 2 or non-insulin-dependent DM is rare in dogs and typically associated with a concurrent insulin-antagonistic condition or treatment such as those outlined below. Obesity-induced insulin resistance has been documented in dogs. However, there are currently no reports of such insulin resistance leading to type DM, as is often the case in humans (the most common type) and even in cats.
What Are the Causes of Insulin Resistance in Dogs?
- Hyperadrenocorticism (Cushing’s disease)
- Diestrus (phase of the ovarian cycle that follows estrus) or pregnancy in females
- Infection (urinary tract infections being the most common)
- Pancreatitis
- Obesity
- Hypothyroidism
- Heart disease
- Chronic kidney disease
Conclusion
Diabetes is a common hormonal condition affecting dogs. Classical signs of this condition include increased water intake, increased urination, increased appetite, and often, accompanying weight loss. Blindness associated with cataract development is another common reason for diabetic dogs to be presented to a veterinary clinic.
Management of diabetes in dogs is centered around insulin administration. In addition to giving insulin, consistency is key when looking after a diabetic dog—keep the diet constant, keep activity levels the same from day to day, and ensure that insulin injections are administered every 12 hours (after confirming that your dog has eaten a full meal).
Unfortunately, especially with improper management of diabetes, there are potentially life-threatening complications such as diabetic ketoacidosis. Hopefully, with various advancements in treatment and monitoring strategies, such complications will become less common.
Featured Image Credit: Helen of Troy, Shutterstock